Rheumatic conditions are under a broad umbrella. Alongside things like rheumatoid arthritis, there is the lesser known Ankylosing Spondylitis (AS), relatively straightforward tendonitis, and more nebulous fibromyalgia. Rheumatic pain is as varied as the conditions that cause it. Although we cannot cure rheumatic conditions, we may be able to help with the symptoms.
Rheumatoid Arthritis (RA)
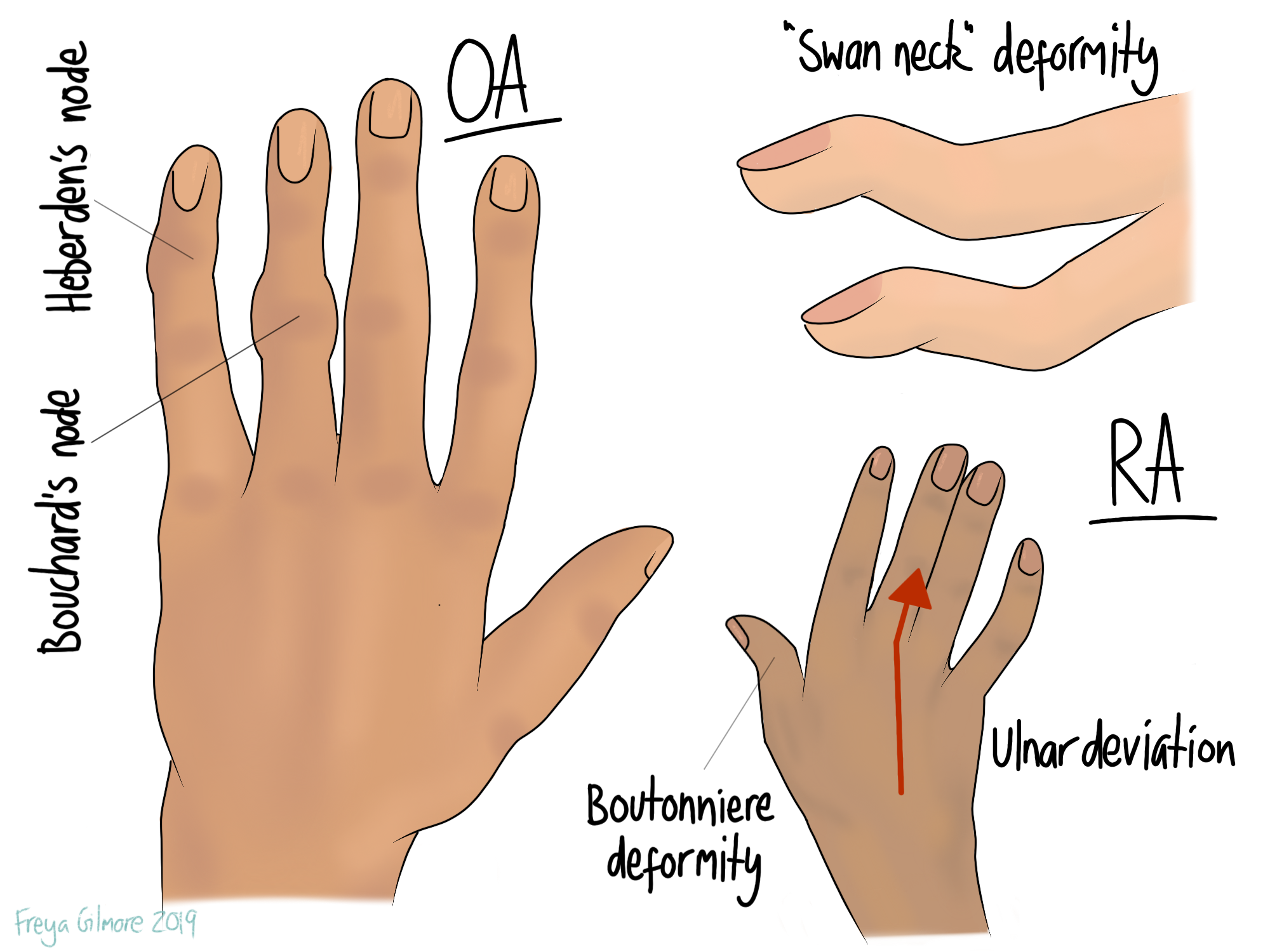
Not to be confused with osteoarthritis (OA), RA is an inflammatory condition that mostly affects the small joints in the hands, feet, and neck. When the hands are affected, the joints can become deformed. Examples include:
- lumps on the knuckles that may be hot and red to begin with, and harden later on
- ulnar deviation of the wrist, where the hands begin to point out (away from the thumbs)
- swan neck deformity, where the last joint in the finger extends and the next flexes
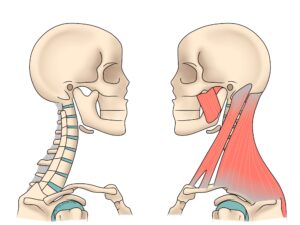
Over time, recurrent flares can cause instability within the joints too. Neck pain may result from damage to the joints themselves, or due to compensation. The neck is a relatively mobile area anyway, so the muscles have to work hard to stabilise if the ligaments become more lax. If the muscles are not strong enough to cope with this demand, new problems can arise. Headaches, shoulder pain, and upper back pain are not unusual.
Our aim in treatment is to help you become as well adapted to your condition as possible. If your neck joints become unstable, we will support you in strengthening the muscles nearby. Occasionally, we see RA patients who have been misdiagnosed. In these cases, we can also help you get the support you need from your GP and rheumatologist.
Ankylosing Spondylitis (AS and AxSpA)
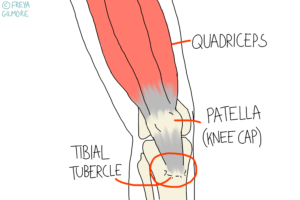
Ankylosing Spondylitis is another inflammatory condition, but this time focused to the lower back. Similarly to RA, there are flares which damage the joints as the body attacks itself. These primarily affect the lower back and pelvis, but can also cause problems in the upper back and in tendons. More specifically, the connection between the tendon and bone is affected- often at the Achilles tendon.
Diagnosis is important to prevent further progression. Rheumatologists can prescribe strong medications to suppress the immune system and limit the attacks on your joints. Unmanaged AS can cause a flattening of the lower back which demands compensation from the neck. This happens as the body repairs itself incorrectly after episodes of AS flares. Rather than repairing the joint as it was before, bone is laid down over the joint itself. This causes stiffness that gets worse with time, and can predispose fractures. The bone over the joints is relatively fragile, so we avoid manipulating in most cases.
AS is poorly diagnosed, taking an average of 8.5 years for diagnosis to be achieved. We see a lot of back pain, so we are in a good position to pick up on cases that aren’t quite right.
Managing Rheumatic Pain
Rheumatic conditions are often inflammatory, which means they need different treatment. Rest can aggravate these conditions, but so can excess activity. Your osteopath can help you find the happy medium and develop an exercise plan. To reiterate: we cannot cure your rheumatic condition, but we may be able to help you manage your pain.