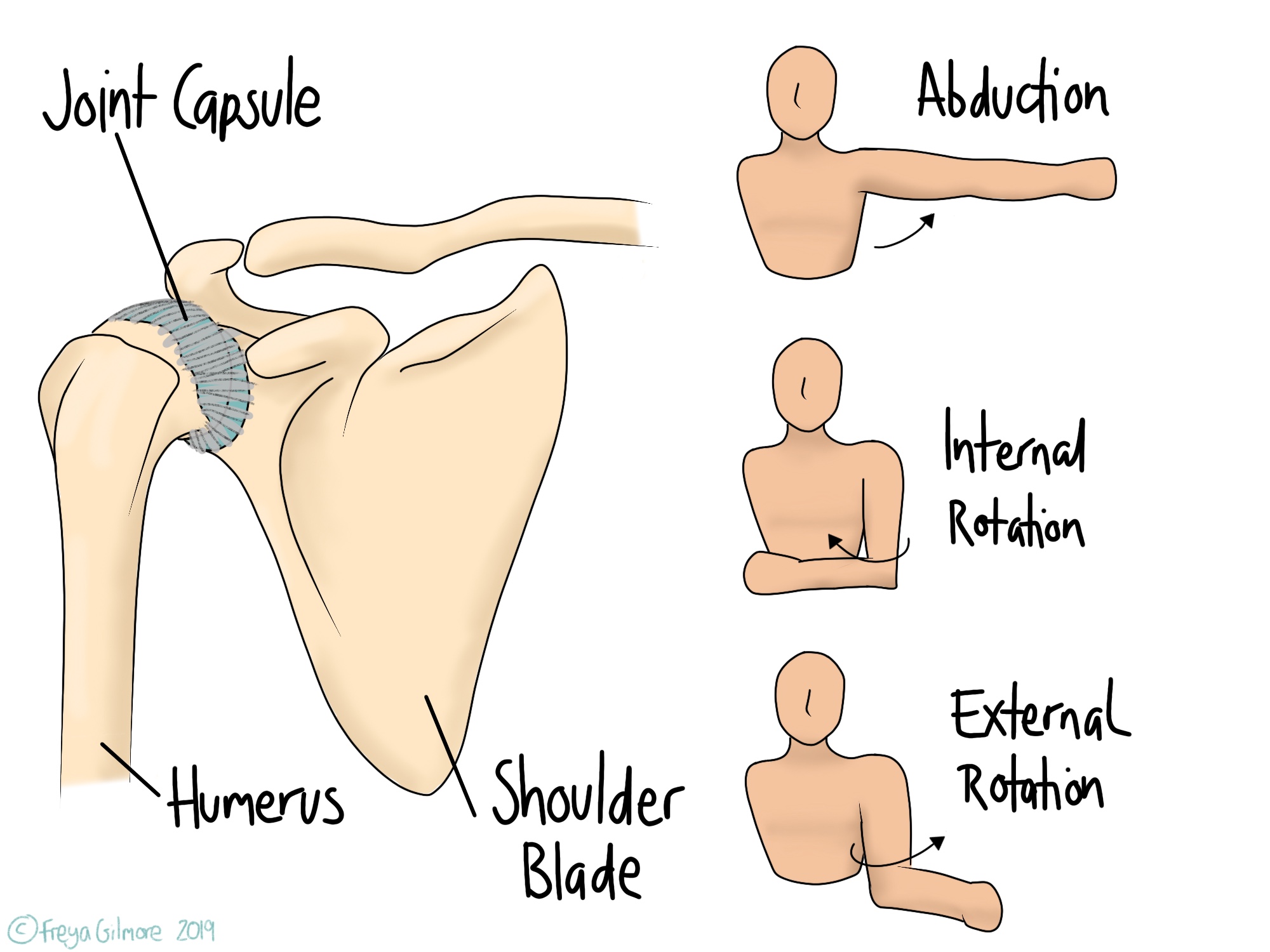
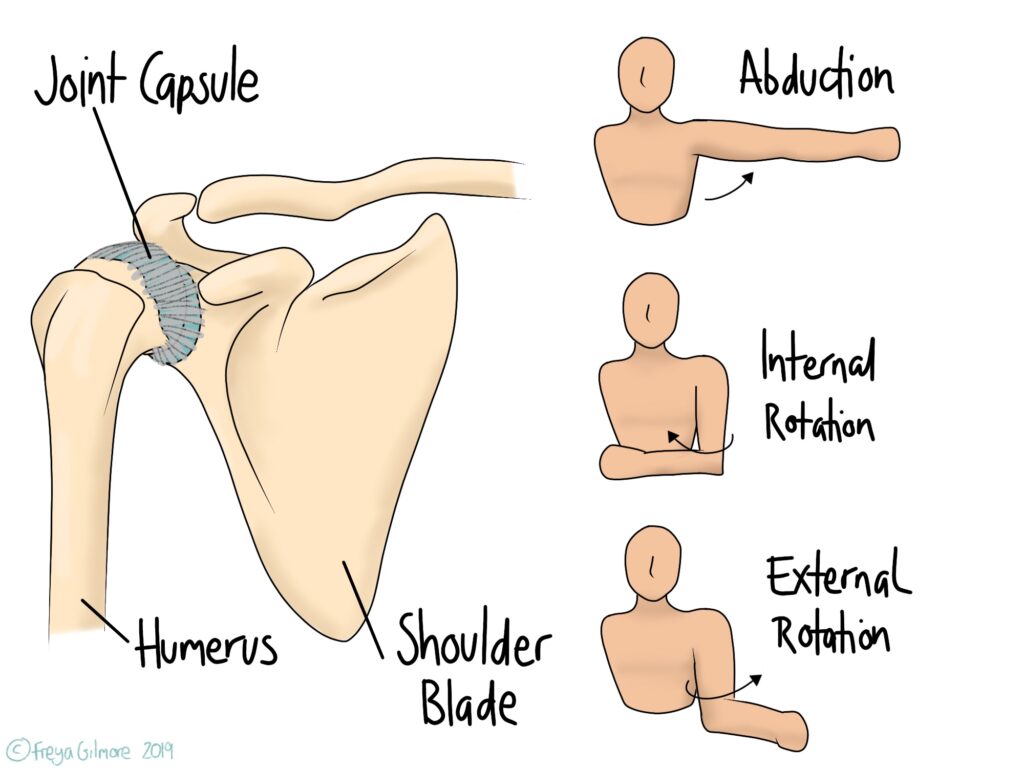
“Frozen Shoulder” isn’t a term for any kind of shoulder pain and restriction. It’s the lay-term for adhesive capsulitis, which means “stuck and inflamed capsule”. The capsule is a tough, fibrous structure that surrounds the ball and socket joint of the shoulder. Its job is to protect the joint and keep it stable, but in frozen shoulder it becomes too restrictive.
What happens in Frozen Shoulder?
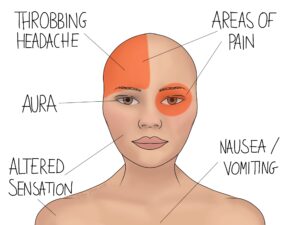
Frozen shoulder starts with shoulder pain that may be quite diffuse or focused around the shoulder tip. This is followed by loss of movement, most noticeably in the ranges shown above. Putting on a coat or fastening a seat belt may become difficult and painful. Thickening or contraction of the joint capsule is what causes this restriction.
There are some risk factors for developing adhesive capsulitis, but not all cases come on for reasons we understand. Periods of immobilisation, such as post-surgery, are a common factor in developing adhesive capsulitis. For this reason it is important to carry out rehabilitation exercises after any surgery. If you have had a shoulder operation and not given exercises, your osteopath can support you with a plan.
There are also more cases of frozen shoulder among people with diabetes, cardiovascular disease, and thyroid issues. The opposite shoulder may develop after the initial side resolves.
The three phases of the condition are: freezing, frozen, and thawing. Each lasts between 4 months and 2 years, and it’s not unusual for it to last around 2 years from first symptom to resolution. During the freezing phase, pain and restricted movement worsen. These plateau during the frozen phase, and improve during the thawing phase.
What can we do?
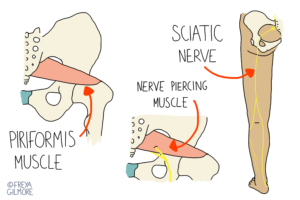
Unfortunately, there is no way to stop a case once it starts. However exercise and manual therapy have been shown to speed up the process. Your osteopath will look at the muscles around the shoulder, especially those around the shoulder blade. We also look at the joints that make up the shoulder, including those either end of the collar bone. Treatment may need to be relatively strong, but we can always adapt this to your needs. It is likely that your body will adapt to the pain and stiffness, so we also want to make sure that the rest of the body is moving well. Changes in posture and movement often affect the neck and upper back, so we like to catch changes there before they cause symptoms.
Self management is important, with movement being the most effective way of managing the condition. Your osteopath will initially give you stretches to do at home. As you progress, these exercises will be updated, and it may be appropriate to start strengthening the shoulder. We tailor your exercise plan specifically to you. We take into account your ability, comfort, and what access to equipment you have.